When it comes to managing anxiety or sleep disorders, the options can seem hectic. Of all the multiple medications available, barbiturates and benzodiazepines are two mainly prescribed drugs. Both play a role in relaxing the central nervous system, but they have prominent differences that warrant understanding.
Barbiturates, a group of sedative-hypnotic drugs, have been in use for decades. They work by depressing the central nervous system, prevailing on sedation, and stimulating sleep. Benzodiazepines, on the other hand, are a class of psychoactive drugs generally prescribed for anxiety, insomnia, and muscle relaxation. They enrich the effects of a neurotransmitter called gamma-aminobutyric acid (GABA), which has a soothing effect on the brain.
Getting the points on the contrasts between barbiturates and benzodiazepines is important for healthcare professionals and patients as well. Factors such as beginning and duration of action, urge for addiction, and side effects vary considerably between the two groups.
In this article, we will scratch into the differences, barbiturates vs benzodiazepines, providing thorough information to help make clever decisions about these medications.
How Barbiturates and Benzodiazepines work

Barbiturates vs Benzodiazepines, both barbiturates and benzodiazepines exercise their effects by expanding the activity of GABA in the brain, but they do so through different mechanisms and imperative sites on GABA receptors.
Barbiturates
- Mechanism of Action: Advanvvs GABA activity by binding to specific receptors, Lessing neuronal activity, resulting in sedation, muscle relaxation, and sleep induction.
- Effects: Produce relaxation, anxiety reduction, sedation, and hypnotic effects, with anticonvulsant properties at higher doses.
- Duration of Action: Fluctuates among short-acting (e.g., pentobarbital) and long-acting (e.g., phenobarbital) compounds, influencing the real-time and duration of effects.
Benzodiazepines
- Mechanism of Action: Upgrades GABA activity by binding to clear-cut receptors, leading to lowered neuronal activity and CNS relaxation.
- Effects: performs anxiolytic, sedative, hypnotic, muscle relaxant, and anticonvulsant effects, generally prescribed for anxiety, insomnia, and muscle cramps.
- Duration of Action: Differs from short-acting (e.g., alprazolam, lorazepam) to long-acting (e.g., diazepam, clonazepam), affecting onset and duration of effects.
Getting thorough with these mechanisms is important for healthcare professionals and patients to make informed decisions about the use of these medications in managing anxiety and sleep disorders.
Medical uses of Barbiturates and Benzodiazepines
Barbiturates vs benzodiazepines, both are used for treating anxiety, sleep disorders, and neurological conditions. Barbiturates provide sedation, anesthesia, and anticonvulsant effects, while benzodiazepines are favored for their anxiolytic, sedative, and muscle relaxant properties. Benzodiazepines are safer than barbiturates, especially with the respiratory depression and overdose. They’re also key in controlling alcohol withdrawal symptoms.
Barbiturates
- Sedation
- Anesthesia induction
- Anticonvulsant therapy
- Short-term treatment of insomnia
Benzodiazepines
- Anxiety disorders (e.g., generalized anxiety disorder, panic disorder)
- Insomnia
- Muscle spasms
- Seizure disorders
- Alcohol withdrawal syndrome
Barbiturates vs Benzodiazepines, both have a scale of medical uses, but benzodiazepines are more prescribed due to their promising safety profile and lesser risk of overdose compared to barbiturates. However, both drug groups carry major risks of tolerance, dependence, and withdrawal symptoms, and their use should be carefully tracked by healthcare professionals.
Side effects and potential risks of Barbiturates and Benzodiazepines

Barbiturates, due to their depressant effects on the central nervous system, can cause drowsiness, dizziness, confusion, and impaired coordination. Additionally, they carry a high risk of tolerance, dependence, and addiction, making them unsuitable for long-term use.
- Drowsiness: Considerable drowsiness spoiling alertness.
- Dizziness: urging lightheadedness, increasing fall risk.
- Confusion: inherent for disorientation, especially at higher doses.
- Impaired Coordination: Affecting motor skills and balance.
- Respiratory Depression: Fatal, slowing of breathing.
- Tolerance, Dependence, Addiction: Risk of tolerance and dependence, leading to addiction.
- Overdose Risk: Narrow therapeutic index, increasing the risk of disastrous overdose.
- Drug Interactions: heavy interactions with various medications, impact productivity.
Benzodiazepines are associated with side effects such as drowsiness, sedation, dizziness, and impaired logical function. Like barbiturates, benzodiazepines carry a threat of tolerance, dependence, and addiction, especially with extended use or high doses.
- Drowsiness: Common sedative effect, impairing cerebral function.
- Sedation: Persuading lethargy and lowered alertness.
- Dizziness: Increasing fall risk, specifically in older adults.
- Impaired Cerebral Function: Memory, attention, and concentration may be affected.
- Tolerance, Dependence, Addiction: Risk of tolerance, dependence, and addiction with prolonged use.
- Overdose Risk: Manipulated risk, especially when combined with other depressants.
- Withdrawal Symptoms: Anxiety, insomnia, tremors, and seizures upon discontinuation.
- Drug Interactions: Interactions with multiple medications, upgrading sedative effects.
It is important to get thorough with these points as they are critical for healthcare professionals and patients when considering the use of barbiturates and benzodiazepines for treatment.
Barbiturates vs Benzodiazepines, their Key Differences in Chemical Structure
Barbiturates and benzodiazepines, both CNS depressants with sedative and anxiolytic effects, differ in their chemical structures. Barbiturates feature a pyrimidine ring fused with a dihydroxy moiety, while benzodiazepines contain a benzene ring fused with a diazepine ring.
Barbiturates
- Contains barbituric acid moiety.
- Core structure: Pyrimidine ring fused with dihydroxy moiety and ketone group.
- Substitutions determine pharmacological properties.
- Characterized by a carbonyl group (C=O) contributing to sedative effects.
- Examples: Phenobarbital, pentobarbital, secobarbital.
Benzodiazepines
- Feature a benzene ring fused with a diazepine ring.
- Core structure: Diazepine ring with two nitrogen atoms.
- Substitutions influence pharmacological properties.
- Characterized by benzene ring contributing to anxiolytic and sedative effects.
- Examples: Diazepam, lorazepam, alprazolam, clonazepam.
Understanding these differences in chemical structure is essential for elucidating the obvious pharmacological properties and clinical effects of these drug classes.
Barbiturates vs Benzodiazepines: Differences in mechanism of action
Both of them act as positive allosteric modulators of GABA-A receptors, but they differ in their specific mechanisms of action. Barbiturates directly upgrade the duration of chloride channel opening and can directly activate GABA-A receptors, while benzodiazepines upgrade the partial parts of GABA for its receptor by binding to an evident allosteric site.
Barbiturates
- Intensify the duration of chloride channel opening.
- Increase chloride ion influx, hyperpolarizing cell membrane.
- Directly activate GABA-A receptors.
- Inhibit excitatory neurotransmission by blocking glutamate receptors.
Benzodiazepines
- Increase the frequency of chloride channel opening.
- Bind to plain benzodiazepine binding sites on GABA-A receptors.
- Increase GABA affinity for its receptor.
- Potentiate GABAergic neurotransmission.
These are the important factors for elucidating the conspicuous pharmacological properties and clinical effects of these drug classes.
Barbiturates vs Benzodiazepines: Variations in potency and duration of action
The variations in potency and duration of action between barbiturates and benzodiazepines have extraordinary clinical implications for their use in medical practice. The choice of medication depends on the specific therapeutic goals, the severity of symptoms, and the desired onset and duration of action.
Potency
- Barbiturates: Differs widely in potency, with phenobarbital being one of the most potent.
- Benzodiazepines: Also Differ in potency, with diazepam considered intermediate and lorazepam/alprazolam being more potent.
Duration of Action
- Barbiturates: Scales from short-acting (secobarbital) to long-acting (phenobarbital).
- Benzodiazepines: Similarly range from short-acting (triazolam) to long-acting (diazepam/clonazepam).
Barbiturates vs Benzodiazepines, diversify in potency and duration of action, they differ in their specific pharmacokinetic properties and mechanisms of action. Understanding these differences is crucial for selecting the appropriate medication for a given clinical indication and minimizing the threat of unfavorable effects.
Barbiturates vs Benzodiazepines: Varied indications and approved uses
Barbiturates vs benzodiazepines, despite sharing some therapeutic properties, have visible indications and approved uses due to differences in their pharmacological profiles.
Barbiturates
- Historically used as sedative-hypnotics, anesthesia induction agents, and anticonvulsants.
- Generally employed for short-term treatment of insomnia, preoperative sedation, and seizure management.
- Phenobarbital, for instance, is used as a long-acting anticonvulsant.
- Lesser use due to safety concerns, including potential for overdose and addiction.
Benzodiazepines
- Extensively prescribed for different anxiety disorders, including generalized anxiety disorder and panic disorder.
- Effective in controlling insomnia, especially for short-term use due to the risk of dependence.
- Also used as muscle relaxants to alleviate spasms and in the treatment of certain seizure disorders.
- Preferred over barbiturates for their safer profile regarding respiratory depression and overdose.
Barbiturates vs Benzodiazepines: Addiction potential and withdrawal symptoms
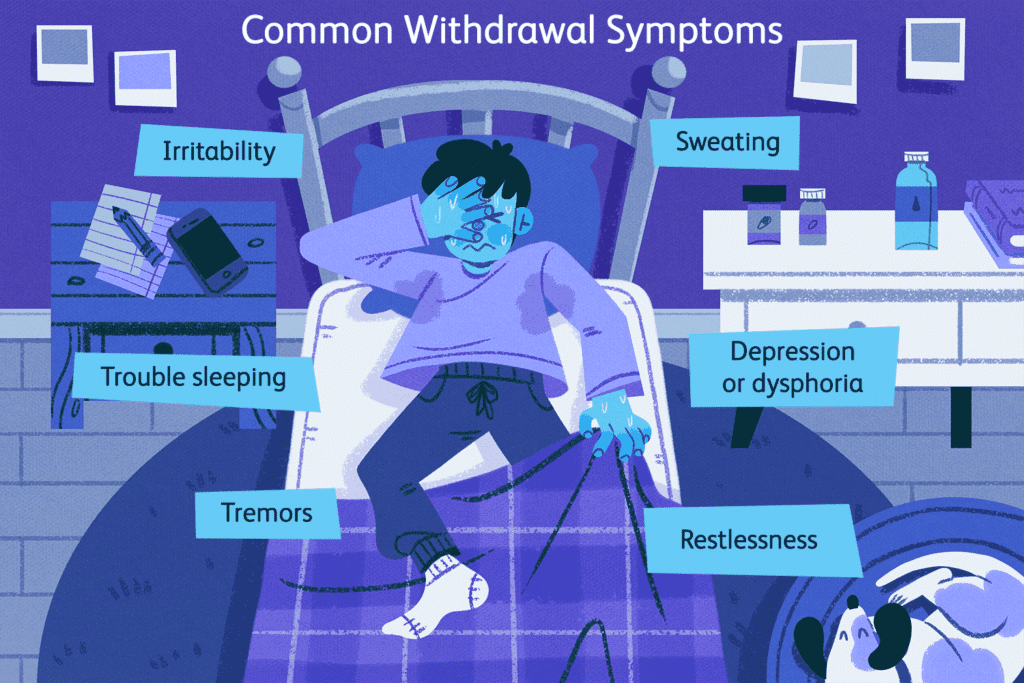
Both barbiturates and benzodiazepines have inbuilt the threat of tolerance, dependence, and addiction, but they vary in their propensity for these issues and the severity of withdrawal symptoms upon discontinuation.
Barbiturates
- High risk of tolerance and dependence, leading to addiction with prolonged use.
- Abrupt cessation or rapid tapering can result in severe withdrawal symptoms, including anxiety, agitation, tremors, seizures, and even life-threatening delirium or coma.
- Due to their narrow therapeutic index, the risk of overdose is significant, especially when combined with other central nervous system depressants like alcohol or opioids.
Benzodiazepines
- While benzodiazepines also carry a risk of tolerance, dependence, and addiction, it is generally lower than that of barbiturates.
- Withdrawal symptoms upon discontinuation can vary depending on factors such as duration of use, dosage, and individual sensitivity.
- Common withdrawal symptoms include rebound anxiety, insomnia, irritability, muscle stiffness, and in severe cases, seizures.
- Tapering off benzodiazepines gradually under medical supervision can mitigate withdrawal symptoms and reduce the risk of rebound anxiety or seizures.
The addiction potential and withdrawal risks associated with barbiturates and benzodiazepines are crucial for healthcare providers when prescribing these medications and for patients undergoing treatment.
FAQs
1. What is the difference between benzodiazepines and barbiturates’ mechanism of action?
Although both categories of drugs are classified as central nervous system depressants, their mechanisms of action differ. Barbiturates function by inhibiting brain and nerve activity through interaction with a particular receptor. Conversely, benzodiazepines operate by enhancing the influence of a neurotransmitter known as gamma-aminobutyric acid (GABA).
2. What is the major advantage of benzodiazepines over barbiturates?
Benzodiazepines and the more recent non-benzodiazepine hypnotics are currently favored over barbiturates for many clinical applications due to their broader therapeutic range, slower development of tolerance, and reduced potential for misuse compared to barbiturates.
3. What is the difference between a depressant and a barbiturate?
Depressants promote sleep, alleviate anxiety and muscle spasms, and inhibit seizures. Barbiturates are considered traditional medications and encompass butalbital (Fiorinal), phenobarbital, Pentothal, Seconal, and Nembutal.
4. What are the four types of barbiturates?
“Ultra brief-duration” barbiturates consist of Methohexital (Brevital), Thiamylal (Surital), and Thiopental (Pentothal). “Brief-duration” and “moderate-duration” barbiturates encompass Pentobarbital (Nembutal) and Secobarbital (Amytal). “Extended-duration” barbiturates include Phenobarbital (Luminal) and Mephobarbital (Mebaral).
Conclusion
The disparities between barbiturates and benzodiazepines underscore the significance of informed decision-making in managing anxiety and sleep disorders. While both drug classes aim to alleviate symptoms by affecting the central nervous system, their mechanisms of action, pharmacokinetic properties, and associated risks vary significantly.
Healthcare professionals and patients alike must grasp these distinctions to ensure safe and effective treatment. From potency and duration of action to addiction potential and withdrawal risks, each factor plays a crucial role in determining the appropriate medication for individual needs.
By staying informed about the nuances between barbiturates and benzodiazepines, healthcare providers can make tailored treatment decisions, minimizing risks and optimizing outcomes for patients. Likewise, patients can actively participate in their treatment journey, making empowered choices under the guidance of their healthcare providers.
In the area of anxiety and sleep disorder management, knowledge truly is power. Let us strive for a collaborative approach that prioritizes safety, efficacy, and patient well-being. Together, we can navigate the complexities of medication therapy with confidence and clarity for sure!